News
Featured article
What are the Different Stages of Prostate Cancer
What Are The Different Stages Of Prostate Cancer And What Do They Mean? A diagnosis of prostate cancer can be devastating, but early diagnosis and selecting the right treatment can improve your prognosis. Not only can the right treatment…
Latest news
How Likely Are You To Develop Prostate Cancer?
How Likely Are You To Develop Prostate Cancer? Prostate cancer is extremely common, and it’s estimated that 1 in 8 men will develop it during…
Busting myths around prostate cancer
Living in an era of information overload is challenging; and in the case of healthcare the sheer quantity of information ranging in…
NanoKnife, enhanced patient choice and the case for prostate cancer screening
Adding NanoKnife to our clinical offer of focal treatments to patients has been eye-opening on a number of levels. Not only has…
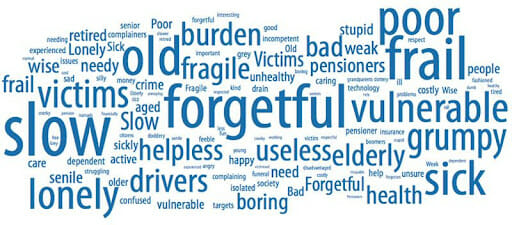
As approaches to ageing change, should we change our approach to diseases of ageing?
As approaches to ageing change, should we change our approach to diseases of ageing? As a clinic we specialise in treating men…
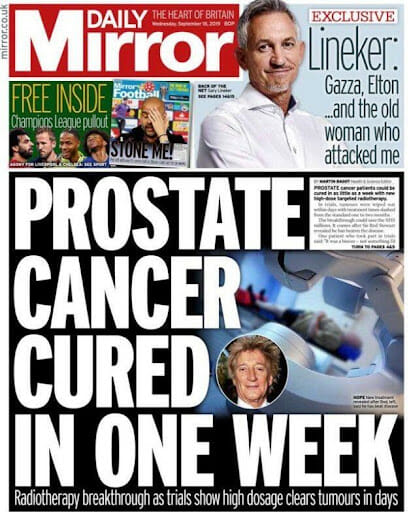
Making sense of media reporting on prostate cancer
Making sense of media reporting on prostate cancer We live in an information-rich time; never before has so much content been available…
A new audio series brought to you by The Focal Therapy Clinic, where our host, Clare Delmar, explores some issues facing men…
Older patients and treatment choice
Two of our consultant urologists, Tim Dudderidge and Raj Nigam, are co-authors on a soon-to-published piece of research into older men’s experience…
Understanding and interpreting clinical research findings – what they mean for you and your decision-making Two recently presented clinical studies highlight important…
Optimising diagnosis and treatment for Prostate Cancer: Why a second opinion can be the best investment you’ll make The majority of men…
Any questions?
Being diagnosed with prostate cancer can be very distressing, and it’s normal to feel anxious, fearful and unsure which treatment to choose. We understand the emotions you may be experiencing and are here to help you to make a confident, informed decision about your care.
If you've got any questions about your prostate cancer diagnosis or want to know more about HIFU or NanoKnife focal don’t hesitate to get in touch with our friendly, knowledgeable team.
Fill in an enquiry form