Reading Time: 7 minutes
Medically Approved by Dr Aqua Asif (May 1st 2025)
Written by Brian Lynch
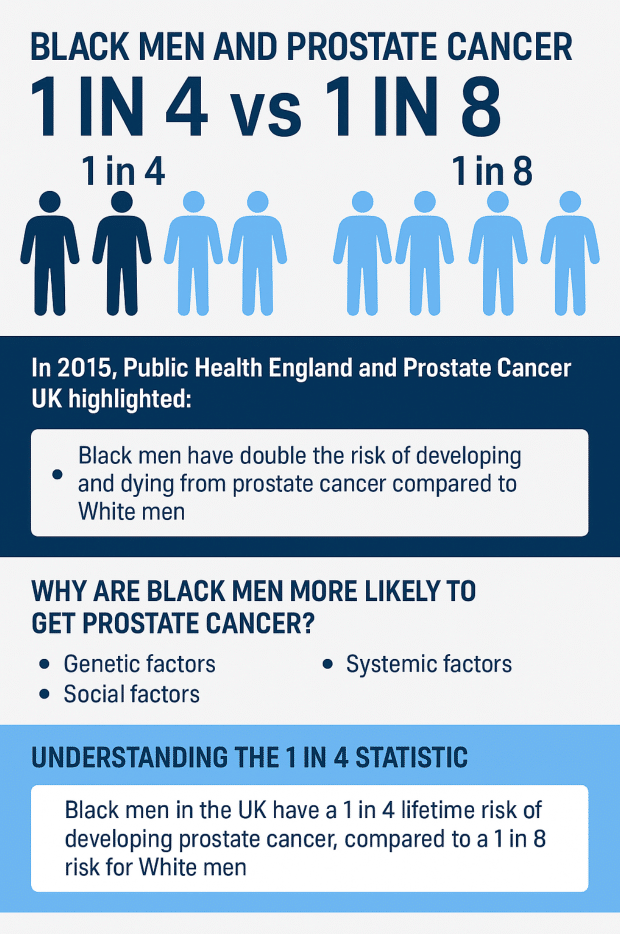
In 2015, Public Health England and Prostate Cancer UK highlighted a stark reality: Black men have double the risk of developing and dying from prostate cancer compared to white men. The lifetime risk was estimated at about 1 in 4 for Black men versus 1 in 8 for white men. Nearly a decade later, this “1 in 4 vs 1 in 8” statistic remains an urgent concern. Unfortunately, despite growing awareness, Black men’s outcomes in prostate cancer have not significantly improved – underlining the need for continued action, research, and support.
Prostate cancer is the most common cancer in British men, and it affects Black men disproportionately. The “1 in 4” risk means that if we followed a large group of Black men from birth to old age, roughly one-quarter of them would be diagnosed with prostate cancer at some point. This elevated risk also translates to higher chances of dying from the disease. These figures are not meant to alarm, but to drive home a critical point: Black men face a uniquely high threat from prostate cancer, and understanding why is key to addressing this health inequality.
Why are black men more likely to get prostate cancer?
There is no single answer, but a combination of genetic, social, and systemic factors is believed to be responsible. On the genetic front, recent research has shed light on inherited risk. Scientists at the Institute of Cancer Research in London co-led a groundbreaking study pooling data from over 200,000 men of diverse ancestries. This global effort identified 86 new genetic variants associated with prostate cancer risk. Many of these variants are more common in men of African descent, helping explain why Black men inherit about twice the average risk of prostate cancer compared to white men. As the ICR study noted, “Black men are known to be at an increased risk of being diagnosed with or dying from prostate cancer… The new analysis… identif[ied] 86 new genetic changes that influence the risk… bringing the total number… to 269”. Each individual genetic change has only a small effect, but combined, these factors can substantially increase risk.
However, genetics are only part of the story. Social and economic factors also play a significant role in health outcomes. Black communities in the UK may face barriers such as lower trust in healthcare providers, experiences of racism or bias, and less access to consistent care. A recent survey found that 69% of Black adults were unaware of their higher risk for prostate cancer, with some Black men reporting having to push to get tested; reflecting possible gaps in awareness and proactive care among both patients and healthcare providers. Socioeconomic disparities can compound this issue, for instance, living in under-resourced areas might mean fewer health outreach programmes and less engagement with GP services. All these factors can delay diagnosis or lead to cancers going unnoticed until they are more advanced.
Genes may load the dice, but issues like unequal healthcare access, cultural stigma around rectal exams or cancer discussions, and not being offered early tests all contribute to the disparity. Understanding these reasons is vital so that tailored strategies, from genetic research to community education, can reduce the risk.
Understanding the 1 in 4 statistic
Black men in the UK face a 1 in 4 lifetime risk of developing prostate cancer, compared to a 1 in 8 risk for white men. Lifetime risk is an estimate based on current data and trends, it doesn’t mean every fourth Black man is destined to get prostate cancer, but it highlights a probability that is significantly higher than average. It combines the influence of genetics, environment, and age. Because prostate cancer mostly affects older men, these statistics assume one lives to a typical old age. If Black men have higher incidence rates at every age, their cumulative risk ends up roughly double that of white men by the end of life.
It’s important to note that this figure was first solidified by a detailed analysis in 2015. That study, conducted by Public Health England and Prostate Cancer UK, combed through cancer registry data to calculate risks by ethnicity. They found Black men in England had about a 29% lifetime chance of a prostate cancer diagnosis (approximately “one in four”), whereas white men’s risk was ~13% (“one in eight”). These findings led to calls for better awareness and possibly targeted screening for Black men. After all, if one group is at such elevated risk, standard one-size-fits-all approaches may not be adequate.
This figure also reflects the impact of long-standing health inequalities in the UK. Many men are still unaware of their increased risk or delay seeking medical advice. Early detection remains one of the most powerful tools to improve outcomes for Black men with prostate cancer.
Gaps in research and diagnosis
Two critical gaps underpin the statistics: under-representation in research and late diagnosis.
Historically, Black men have been under-represented in prostate cancer trials. When treatments and screening tools are developed mostly on white populations, we might miss important differences in how Black men respond or what approaches work best. Low participation often stems from medical mistrust, lack of outreach, or eligibility criteria that unintentionally exclude minority patients. The result is that evidence specific to Black men’s needs has lagged behind.
At diagnosis, Black men not only get prostate cancer more often, they are too often diagnosed later. The latest National Prostate Cancer Audit shows Black men have higher rates of stage 3–4 disease at diagnosis than any other ethnic group. Lower uptake of PSA testing and inconsistent GP practice are big factors. The UK has no national screening programme as of yet; men are usually tested only after discussing risk or symptoms with their GP. If clinicians are not proactively raising the issue, opportunities for early detection can be missed, particularly when guidelines treat Black men the same as average-risk groups.
Addressing these gaps requires targeted action: inclusive research, proactive testing for high-risk patients, and empowering Black men to request tests without push-back. By prioritising research on Black men’s experiences and outcomes, and collaborating with Black community groups, we can start to plug the holes in the system.
The role of awareness and early detection
Early detection can be life‑saving, and awareness is key. The stories of Delroy Wright and Marcus McKenzie illustrate this.
Delroy went to his GP for a check‑up and specifically asked about prostate cancer because of his risk. Although initially reluctant about a rectal exam, he persisted. His first PSA was slightly high but he was told “don’t worry”; six months later it rose further, prompting an MRI and biopsy. Because his cancer was caught before it spread, Delroy could start on active surveillance rather than immediate surgery.
Marcus was already aware of his heightened risk and requested annual PSA tests. When a GP questioned their value, he insisted, citing his ethnicity. His diligence meant his cancer was also caught early, and he remains on surveillance with excellent quality of life.
Their experiences show how self‑advocacy and early testing open up more options. When caught early, prostate cancer can often be managed conservatively or with less invasive treatments. For inspiration, many men share their journeys in our prostate cancer treatment success stories, proof that early action makes a real difference.
Community campaigns making a difference
Community-led campaigns are helping bridge the gap in awareness and early diagnosis. Wessex Cancer Alliance partnered with local organisations to create podcasts, online support groups, and local outreach. Efforts like this make information about prostate cancer more personal, relatable, and easier to access.
One of the most powerful advocates is Errol McKellar, a former football coach and prostate cancer survivor. Following his diagnosis, he launched the Errol McKellar Foundation to raise awareness in Black communities. His story has inspired many men to take their health seriously and get tested early.
The foundation now provides mobile PSA testing across the UK. These services bring checks to familiar settings like workplaces, leisure centres, and community clubs. These efforts are already increasing early‑stage diagnoses among Black men, showcasing culturally relevant outreach is effective.
What still needs to change
Systemic change has been slow. Sir Michael Marmot’s reviews on health inequalities show gaps persist, and the NHS Race and Health Observatory has called for radical action to tackle ethnic disparities. NHS England’s CORE20PLUS5 programme now prioritises early cancer diagnosis in deprived and minority communities, but implementation on the ground must accelerate.
Key priorities include risk‑based testing guidelines, greater inclusion of Black men in research, and culturally competent healthcare so Black men feel heard and respected. The odds have been stacked against Black men for too long; concerted action is needed to change that.
Where to get support and information
Black men facing prostate cancer need access to trusted information and supportive care. The Focal Therapy Clinic provides second opinions and advanced, minimally invasive treatments such as HIFU and NanoKnife. These approaches aim to treat only the cancer while preserving healthy tissue and quality of life.
Community-led initiatives offering mobile PSA testing are expanding across the UK. These services help men get tested in places they already visit, making early detection more accessible. Support groups and awareness campaigns also play a key role in helping men talk openly about prostate cancer and share their experiences.
Online platforms, local events, and charity networks offer additional guidance and emotional support. Partners and families can also benefit from these resources, especially when navigating a diagnosis. Access to accurate information and early testing is essential to improving outcomes around prostate cancer black men face today.
To help men understand their options, The Focal Therapy Clinic also offers a detailed focal therapy treatment selection guide. This resource explains how different treatments work and who they may be suitable for. It’s a useful starting point for anyone exploring less invasive options.
In summary, support is available at every stage, from risk assessment to choosing treatment and living life after cancer. Being informed, getting the right support, and having access to the best options are your rights.
References
Cancer Research UK. (2024). Prostate cancer incidence statistics. Retrieved from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/prostate-cancer
Public Health England. (2015). Black men have twice the risk of prostate cancer compared to white men. Retrieved from: https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-015-0405-5
Institute of Cancer Research. (2024). Study sheds light on genetic basis of Black men’s higher prostate cancer risk. Retrieved from: https://www.icr.ac.uk/about-us/icr-news/detail/study-sheds-light-on-genetic-basis-of-black-men-s-higher-prostate-cancer-risk
National Prostate Cancer Audit. (2025). State of the Nation Report 2025. Retrieved from: https://www.npca.org.uk/reports/npca-state-of-the-nation-report-2025
NHS Race and Health Observatory. (2024). Ethnic inequalities in healthcare. Retrieved from: https://www.theguardian.com/society/2022/feb/13/radical-action-needed-to-tackle-racial-health-inequality-in-nhs-says-damning-report
Sir Michael Marmot. (2023). Interview: The UK’s persistent health inequality. Retrieved from: https://www.theactuary.com/2023/05/04/interview-sir-michael-marmot-uks-persistent-health-inequality
NHS England CORE20PLUS5. (2024). Core20PLUS5 – an approach to reducing healthcare inequalities. Retrieved from: https://www.england.nhs.uk/about/equality/equality-hub/national-healthcare-inequalities-improvement-programme/core20plus5/