MRI Imaging for Prostate Cancer
Magnetic resonance imaging (MRI) is an important tool in diagnosing and treating prostate cancer. It uses magnetism and radiowaves to create a picture of what’s inside your body. A positive biopsy is required to definitively diagnose prostate cancer.
MRI imaging aids the precise targeting of areas for focal therapy. Recent developments in MRI technology have allowed radiographers to create more accurate scans. This incudes the development of multiparametric MRI scans (mpMRI).

What is a Multiparametric MRI (mpMRI) scan for prostate cancer?
An mpMRI (multi-parametric MRI) is a highly detailed imaging test that helps identify clinically significant prostate cancer more accurately than a biopsy alone. It also reduces unnecessary biopsies by 25% and improves biopsy sample accuracy.
At The Focal Therapy Clinic, we use your mpMRI results to determine if you're suitable for focal therapy. During the scan, a contrast agent is used to make images clearer, helping us see if cancer is confined to the prostate or has spread.
What to expect when getting your MRI scan
- You may be asked to change into a hospital gown or keep your clothes if they don’t have metal (zips, clips).
- Remove jewellery, body piercings, and your watch.
- Empty pockets of coins and keys.
- You can bring a friend or relative, but they must also remove any metal.
- You'll lie on your back on a couch that slides into the MRI machine.
- A contrast dye may be injected into your arm to enhance images of the prostate.
- Possible mild side effects from the dye: nausea, headache, warmth, metallic taste, dizziness.
- Stay as still as possible (scan takes about 10 minutes).
- The radiographer will monitor you throughout, and you can communicate via an intercom.
- You may be asked to hold your breath at times.
- The MRI machine makes a loud clanging sound—headphones will be provided for hearing protection.
Getting the results
A radiologist will review your MRI images and assign a score from 1 to 5, known as your PI-RADS or Likert score. This score indicates the likelihood of cancer in your prostate, with 1 being low risk and 5 being high risk.
Fusion MRI
Fusion MRI is an advanced technique that combines MRI scans with live ultrasound to guide prostate cancer treatments.
In a fusion MRI, our expert radiographer marks your prostate, your tumour and lesions, your seminal vesicles and your urethra on your scan results. In a fusion biopsy, a grid is also added. During your biopsy, your MRI scan is overlayed onto your live ultrasound, and a grid-shaped needle guide is used to accurately sample the target area. With a transperineal fusion MRI-guided biopsy, there is very little downtime or soreness afterwards, and it’s much more accurate in confirming a suspected diagnosis of prostate cancer.
During fusion focal therapy, the MRI scan is overlayed onto your live ultrasound and this is used to guide your treatment; for HIFU, this is an ultrasound probe, and for NanoKnife, it is needles. This allows your surgeon to target your tumour very accurately, increasing the effectiveness of your treatment and reducing the risk of damaging any other tissue.
- Improved Tumour Detection – More accurate than ultrasound alone
- Greater Targeting Precision – Helps specialists precisely pinpoint tumours
- Reduces Risk of Missing Cancerous Tissue – Ensures comprehensive tumour destruction
How Is an Ultrasound-MRI Fusion Prostate Biopsy Done?
You first receive a prostate MRI. The radiologist reviews the images for areas that are suspicious for prostate cancer.
Next, doctors perform an ultrasound test. Your doctor provides local anesthesia for your comfort and inserts a small ultrasound probe into the rectum.
The fusion biopsy technology combines your MRI images with the ultrasound image in real time. This fusion (blending) of images creates a clearer picture to pinpoint any suspicious areas in the prostate.
Your doctor uses the ultrasound and prostate MRI images to collect the prostate biopsy (tissue sample) with a needle. Only urologists with special training and knowledge of prostate cancer perform this procedure.
“I didn’t have a multi parametric [MRI]. It was a conventional imaging, and that didn't show anything on the normal MRI…..it was from the biopsy how I was diagnosed.The biopsy showed that I had prostate cancer, and fortunately, because I caught it early, it was Gleason six, which is the early stages.”
Alphonso Archer
The Focal Therapy Clinic patient
Questions to ask your doctor

Are You a Good Candidate for HIFU (High-Intensity Focused Ultrasound)?
- Your cancer is intermediate risk (usually Gleason 3+4 or 4+3).
- The cancer is localised (hasn’t spread outside the prostate).
- Your PSA is under 15–20 ng/mL.
- You are expected to live at least 8–10 more years.
- The cancer is in one main spot and small enough to target.
Note: HIFU is not usually used for very low-risk or very high-risk cancer. It aims to treat the cancer while keeping side effects like incontinence or erection problems low.
"I had the HIFU procedure with Tim Dudderidge and was very happy with the results... I have absolutely no incontinence and I'm fully sexually active without any side effects."
“Focal HIFU treats cancer with lower side effects.”
HIFU is available at the Focal Therapy Clinic in the UK. It is one of the leading centres for focal therapy, including HIFU, NanoKnife, and Cryotherapy. The team includes top urologists like Mr. Tim Dudderidge, Mr Marc Laniado, Mr Raj Nigam and Mr Alan Doherty who have treated over 2,000 patients successfully.
Patient quote: "I had the HIFU procedure with Tim Dudderidge and was very happy with the results." – Graham Pipe, FTC HIFU patient.HIFU targets only the cancer, not the whole prostate. This means fewer side effects like leaking or erection problems compared to surgery or radiotherapy. NanoKnife is also precise and may preserve erections slightly better, especially in tricky cancer locations.
Patient quote: "I have absolutely no incontinence and I'm fully sexually active without any side effects." – Graham Pipe, HIFU patientSurgeon quote: "Focal HIFU kills cancer with minimal side effects. It preserves sexual function reliably." – Mr. Alan Doherty
HIFU can be safely repeated if the cancer comes back in the treated area. Studies show about 15 to 20% of men may need a second round, and it usually works well. Follow-up scans and biopsies help decide if another treatment is needed.
Urologist quote: “Focal HIFU lets us hit the cancer without harming the rest of the prostate.” – Mr. Raj NigamFor men with intermediate-risk, localized prostate cancer, HIFU has a success rate of about 88% at 5 years—meaning no need for surgery, radiation, or further treatment. Side effects are usually mild: 2% need a pad for leaks for a short time, and 90%+ men keep erections, especially if function was good before treatment.
Urologist quote: “HIFU preserves sexual function reliably.” – Mr. Alan DohertyPatient quote: “I have no incontinence and full sexual function after HIFU.” – Nigel Harris, FTC patient
- PSA tests every 3 months for the first year
- MRI scan at 12 months
- Biopsy only if the MRI scan indicates an area of concern
- Regular checks for urinary or sexual function
This helps catch any signs of cancer coming back early.
Urologist quote: “Monitoring side effects and recurrence rates is a key part of our research” – Mr. Marc LanaidoFrequently asked questions
- T2-weighted images: Cancerous areas may look darker than normal prostate tissue.
- Diffusion-weighted imaging (DWI): Cancerous regions may restrict water movement, appearing brighter.
- Contrast-enhanced imaging: Cancerous tissue may show increased blood flow, enhancing its visibility.
- Score 1 or 2: Unlikely to have significant cancer.
- Score 3: Uncertain; further tests may be needed.
- Score 4 or 5: Likely to have significant cancer.
Learn more about Focal Therapy and Prostate Cancer
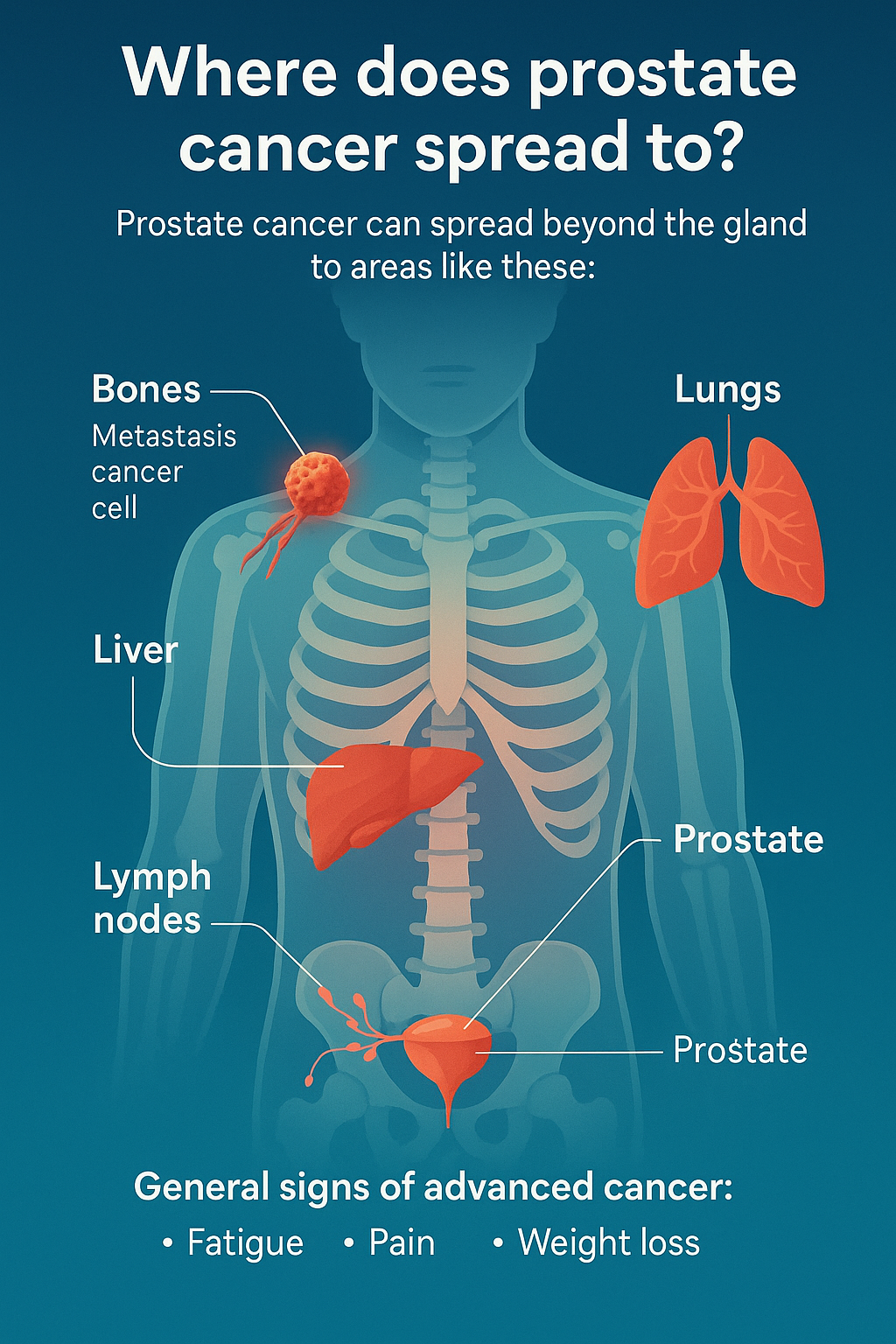
Where does prostate cancer spread to?
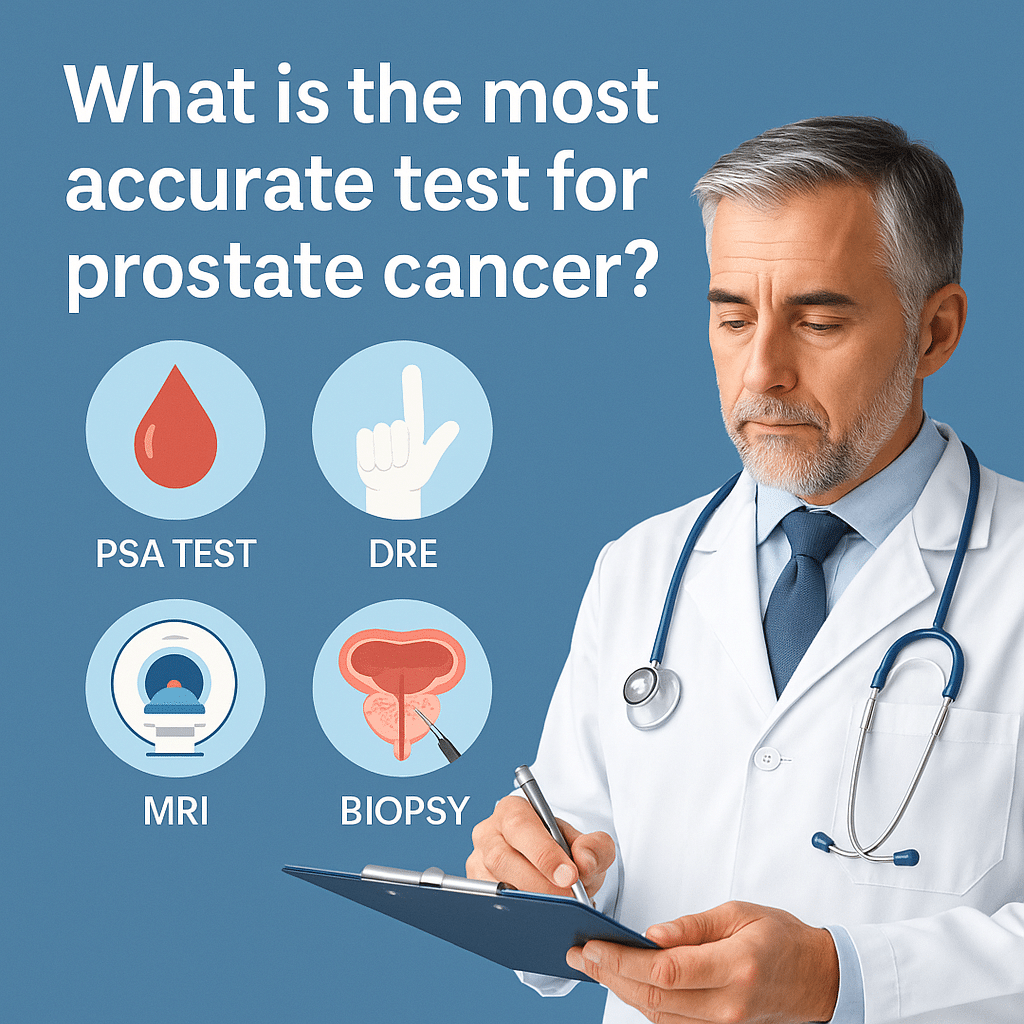
What is the most accurate test for prostate cancer?
What is a PSMA PET scan for prostate cancer?
Any questions?
If you’ve got any questions about your prostate cancer diagnosis or want to know more about HIFU or NanoKnife, don’t hesitate to get in touch with our friendly, knowledgeable team.
Contact the team
Reference List
Ahmed HU et al. (2015). Focal therapy for localized prostate cancer: a systematic review of the literature. Nature Reviews Urology.
Ganzer R, Fritsche HM, Brandtner A, et al. (2017). Five-year outcome of HIFU treatment for localized prostate cancer. Urologia Internationalis.
The Focal Therapy Clinic – Prostate Cancer Treatments (Internal Resource).
NHS Resources on Prostate Cancer (Internal/External Resource).