Over the last few weeks, we’ve begun to see some new questions emerging around Active Surveillance (AS), arising from four areas:
- The completion of over 800 interviews with patients who have come to the Focal Therapy Clinic, conducted over the last 8 months.
- 2 recent clinical studies led by Imperial College London.
- More evidence on mental health support needed for men with prostate cancer during the pandemic and, in particular, for those on AS.
- More evidence on the experience of black men and AS.
All men with prostate cancer have the right to choose the treatment best suited for them, and with this right to choose comes a clinical obligation to provide information and counsel. New information and evidence often emerge in bursts, and this recent burst has placed an emphasis on questions that all men and their clinicians need to raise when considering AS.
1. Clinical studies:
Two studies have been published within the last month that raise new questions about AS. The first compared oncological outcomes of men undergoing focal therapy versus men undergoing radical prostatectomy over an eight-year period, and the results showed the outcomes to be very much the same.
Question: Will this new evidence support FT as a real alternative not only to RP but to AS as well?
TFTC Consultant urologist Alan Doherty thinks so:
“Focal HIFU does give you this great ability to say to a patient, why would you just watch this thing? I can understand why you might not want to go all the way to have a radical treatment that will give you a good chance of curing you but nevertheless will give you quite a few side effects. And why not choose the middle ground? And as technologies are getting better and MRIs are getting better, you are able to sort of keep a very close eye on the prostate where you’ve treated the target lesion. That’s very exciting and very powerful. It’s giving patients another option and I think that’s fantastic.”
The second study showed results on Prostagram, an imaging-based screening programme for prostate cancer developed by Imperial College London.
Prostagram was tested on over 400 men across the UK, comparing different ways of scanning the prostate and optimising a technique, which led to very encouraging results — Prostagram picked up twice as many prostate cancers compared to the standard PSA (prostate-specific antigen) blood test.
Question: What effect will the eventual adoption of Prostagram have on treatment for prostate cancer?
Alan Doherty thinks it will have a significant effect:
“The adoption of Prostagram will increasingly reinforce the acceptance of focal therapy and the rejection of Active Surveillance, as target lesions are identified early, getting more precisely determined as the diagnostic pathway unfolds and non-invasive curative treatment is available.”
2. Comments from our Patients
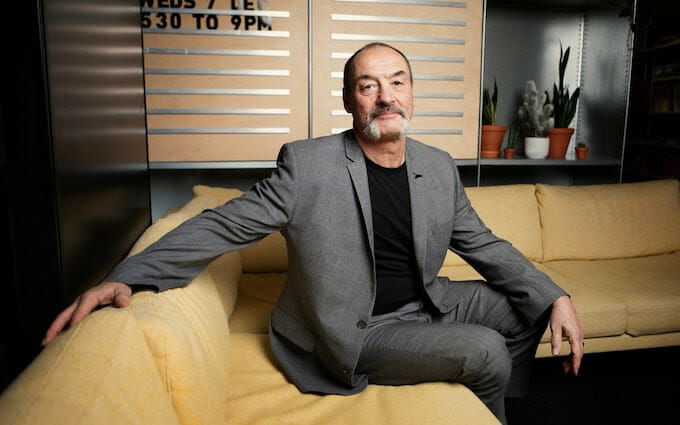
A significant number of patients interviewed by TFTC over the last six months commented on their experiences with AS. One patient stood out in his openness and honesty.
Perry Letcher talked openly about his short-lived experience with AS. Initially, he was positive about it, “at the time, I was relieved because I had been worried that I had a life-threatening illness”, he told us.
“And I was suddenly told, actually, this isn’t, in your case, a life-threatening illness. This is a low grade, low volume tumour. And a lot of people have this. You’re a bit too young in some respects to be getting this. And it is something we need to keep an eye on. And at the time, you know, when I was told active surveillance, that seemed perfectly logical and I was perfectly happy about it.”
Yet soon after Perry felt differently, struggling with the mental and emotional strain of his diagnosis which he began to feel was not treated at all v actively monitored.
TFTC Consultant Raj Nigam feels strongly about this.
“The criteria for AS ignores mental well-being” says Raj. “Having gone through the process of diagnosis, and then being told he doesn’t need to do anything and yet he has cancer, is too much for some men. They simply find this hard to accept, and they cannot live with the not knowing”
Question: Do patients undergoing AS need more support in their overall well-being and ongoing counselling on their suitability?
Perry thinks so:
“I think one of the big issues with Active Surveillance is that one’s perception changes over time…and I think that it’s very easy for the NHS to say, you know, he’s on active surveillance and that’s OK and we’ll just leave it, not realising that that person can have massive changes in their own feelings about how it goes”.
3. Focus on Mental Health
COVID-19 has placed a spotlight on mental health in the general population, and in the case of men with a prostate cancer diagnosis, either undergoing or awaiting treatment, it has underscored the importance of integrating their mental health needs into the management of their disease. A recent study at St George’s Hospital London outlined how this might be done:
“as a clinical community we need to drive a shift in culture towards measurement of patient quality of life as a marker of treatment effectiveness. It appears that despite recent developments in cancer treatment, many of which have improved patient survival, the clinical community has been rather myopic in failing to adequately consider how investing in the mental health of cancer patients can improve patient experience, quality of life, functioning, and even engagement. This involves doing things differently, namely thinking innovatively and more effectively integrating mental health and psychological wellbeing into routine cancer services”.
There has been an increase in men going on AS programmes over the last year, as other treatments are restricted due to Covid. As TFTC Consultant Marc Laniado comments,
“Being on active surveillance, a lot of people would get worried that they’re going to miss the opportunity to have a successful treatment. And that’s obviously not very nice.”
Question: Is the mental health of men undergoing AS often compromised, and are some more at risk than others?
According to Willie Underwood, a urologist in Buffalo, New York, who was diagnosed with prostate cancer at age 48, the answer is yes, and black men are particularly vulnerable.
“If a man will be in ‘PSA prison’ every time he gets his PSA checked, he’s going to go through mental anxiety and living hell, then he might as well get treatment because you’ll be able to go on with the rest of your life and feel more comfortable.”
Dr Underwood, who is black, cites evidence that black men are also at higher risk of depression and anxiety after a prostate cancer diagnosis. More on this below.
4. Experience of Black Men
A recent opinion piece in a popular medical journal referred to a study published late last year which tested the hypothesis that African-American men undergoing AS are at significantly higher risk of disease progression, metastases, and death from prostate cancer compared with non-Hispanic white men.
The researchers found that 59.9% of African-American men experienced disease progression compared with 48.3% of white men. In addition, 54.8% of African Americans required treatment compared with 41.4% of white men. Both were statistically significant increases.
Dr Underwood was baffled by what he perceived to be mixed messages. on one hand, they say that AS is good for Black men, and on the other, they express the accepted wisdom that prostate cancer in Black men is biologically different and usually more aggressive than in white men.
Question: Should black men undergo AS treatment at all?
Dr Underwood suggests not:
“If Black men have more aggressive cancer, then why would you treat them less aggressively?” Underwood asks. “If they’re not like white men, why would you treat them like whites? So, on the one hand, you say they are, but on the other hand you’re saying they’re not.”
His colleagues add that Black men tend to resist AS, suggesting that the idea of coexisting with prostate cancer has been a hard sell in communities of all colours in which doctors have promoted the mantra of “early detection saves lives”.
They added that there has been a historical mistrust of the medical community and researchers in many black communities, which is also coming to light in the deployment of COVID-19 vaccines.
What are your experiences with AS? We’d love to hear from you.